Differentiation of acute and chronic vertebral compression
$ 25.50 · 4.9 (541) · In stock
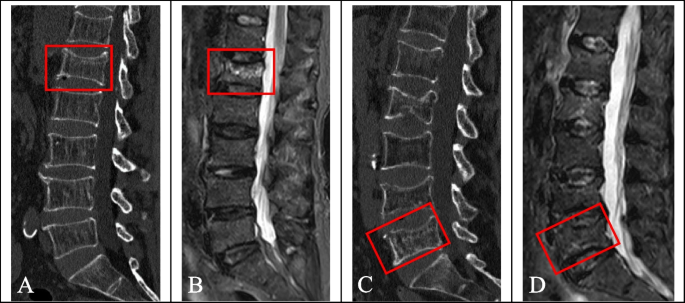
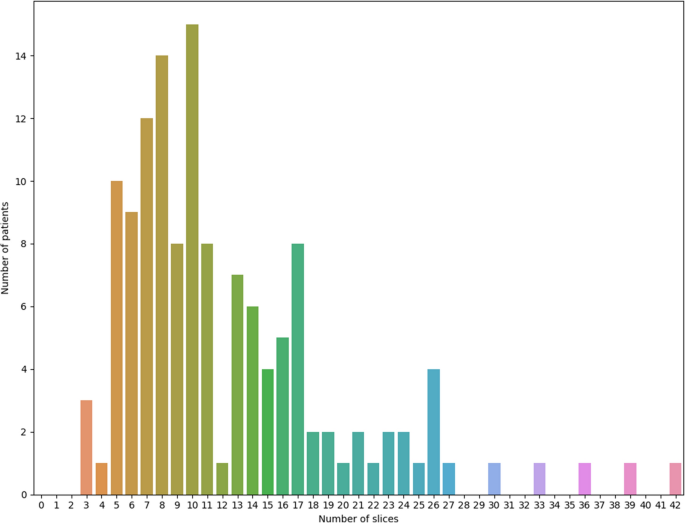
Background We evaluated the diagnostic efficacy of deep learning radiomics (DLR) and hand-crafted radiomics (HCR) features in differentiating acute and chronic vertebral compression fractures (VCFs). Methods A total of 365 patients with VCFs were retrospectively analysed based on their computed tomography (CT) scan data. All patients completed MRI examination within 2 weeks. There were 315 acute VCFs and 205 chronic VCFs. Deep transfer learning (DTL) features and HCR features were extracted from CT images of patients with VCFs using DLR and traditional radiomics, respectively, and feature fusion was performed to establish the least absolute shrinkage and selection operator. The MRI display of vertebral bone marrow oedema was used as the gold standard for acute VCF, and the model performance was evaluated using the receiver operating characteristic (ROC).To separately evaluate the effectiveness of DLR, traditional radiomics and feature fusion in the differential diagnosis of acute and chronic VCFs, we constructed a nomogram based on the clinical baseline data to visualize the classification evaluation. The predictive power of each model was compared using the Delong test, and the clinical value of the nomogram was evaluated using decision curve analysis (DCA). Results Fifty DTL features were obtained from DLR, 41 HCR features were obtained from traditional radiomics, and 77 features fusion were obtained after feature screening and fusion of the two. The area under the curve (AUC) of the DLR model in the training cohort and test cohort were 0.992 (95% confidence interval (CI), 0.983-0.999) and 0.871 (95% CI, 0.805-0.938), respectively. While the AUCs of the conventional radiomics model in the training cohort and test cohort were 0.973 (95% CI, 0.955-0.990) and 0.854 (95% CI, 0.773-0.934), respectively. The AUCs of the features fusion model in the training cohort and test cohort were 0.997 (95% CI, 0.994-0.999) and 0.915 (95% CI, 0.855-0.974), respectively. The AUCs of nomogram constructed by the features fusion in combination with clinical baseline data were 0.998 (95% CI, 0.996–0.999) and 0.946 (95% CI, 0.906–0.987) in the training cohort and test cohort, respectively. The Delong test showed that the differences between the features fusion model and the nomogram in the training cohort and the test cohort were not statistically significant (P values were 0.794 and 0.668, respectively), and the differences in the other prediction models in the training cohort and the test cohort were statistically significant (P < 0.05). DCA showed that the nomogram had high clinical value. Conclusion The features fusion model can be used for the differential diagnosis of acute and chronic VCFs, and its differential diagnosis ability is improved when compared with that when either radiomics is used alone. At the same time, the nomogram has a high predictive value for acute and chronic VCFs and can be a potential decision-making tool to assist clinicians, especially when a patient is unable to undergo spinal MRI examination.

Differential diagnosis of vertebral compression fracture using in-phase/opposed-phase and short TI inversion recovery imaging

Management of vertebral compression fractures - Sports Medicine Review

Sub end-plate compressive fracture in a 60 year old female. (a

Fast kilovoltage (KV)-switching dual-energy CT virtual noncalcium

Differentiation of acute and chronic vertebral compression fractures using conventional CT based on deep transfer learning features and hand-crafted radiomics features, BMC Musculoskeletal Disorders

Lumbar Compression Fracture: Practice Essentials, Pathophysiology, Epidemiology
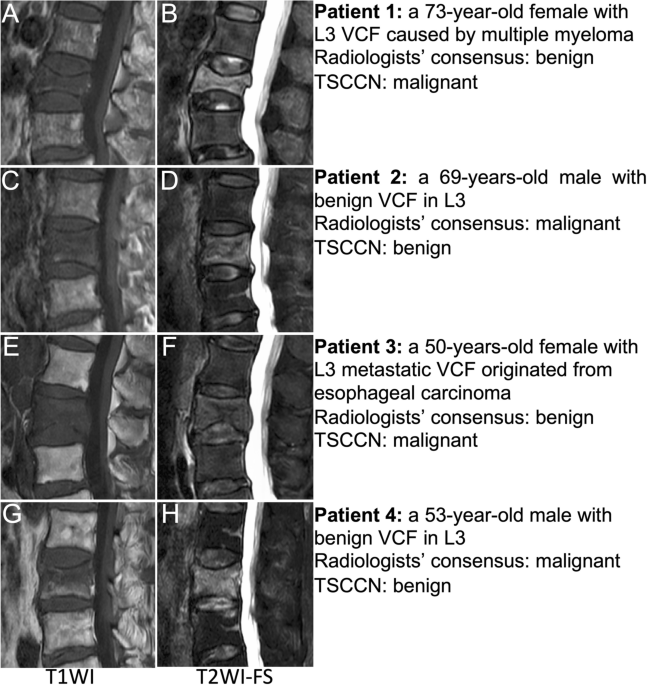
Benign vs malignant vertebral compression fractures with MRI: a

PDF] Radiologic Evaluation of Chronic Vertebral Compression
text {DRTOP}$$ : deep learning-based radiomics for the time-to

Radiographic assessment of acute vs chronic vertebral compression fractures
Vertebral Compression Fractures – Symptoms, Complications, Diagnosis and Treatments
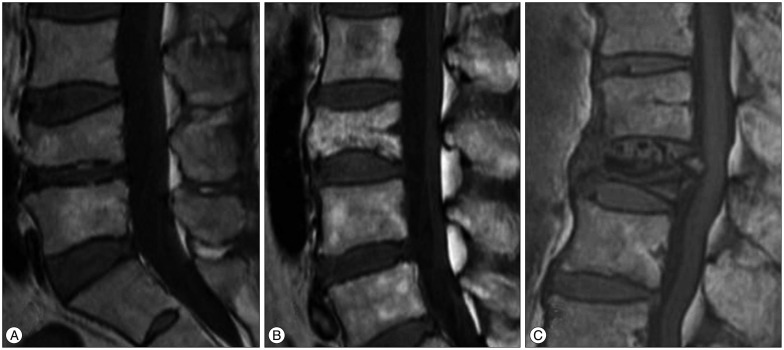
Journal of Korean Neurosurgical Society

Benign vs malignant vertebral compression fractures with MRI: a
